Future-Proofing California’s Community Health Programs
The Growing Challenges for Community Health Providers in California
California’s community health system is at a crossroads, with a rapidly evolving policy environment, growing financial uncertainty, and increasing administrative burdens threatening the sustainability of vital programs. CalAIM, Medi-Cal-funded initiatives, and other state-supported programs were designed to enhance whole-person care, but providers now face new operational complexities that can hinder their ability to deliver impactful services.
The Current Landscape: Challenges Facing Providers
Funding Cuts & Budget Constraints: Changes at the federal and state level threaten Medi-Cal and grant-based funding streams, leaving providers in a financially precarious position【2】
Administrative Burden & Compliance Complexity: The extensive reporting requirements from MCPs, DHCS, and grant agencies demand significant staff time and resources to maintain compliance【3】
Workforce Shortages & High Caseloads: Rising demand for services without an increase in available workforce leads to provider burnout and limits program capacity【4】
Fragmented Data & Inefficient Coordination: Lack of interoperability between systems used by MCPs, CBOs, and health providers leads to redundant efforts and missed care opportunities【5】
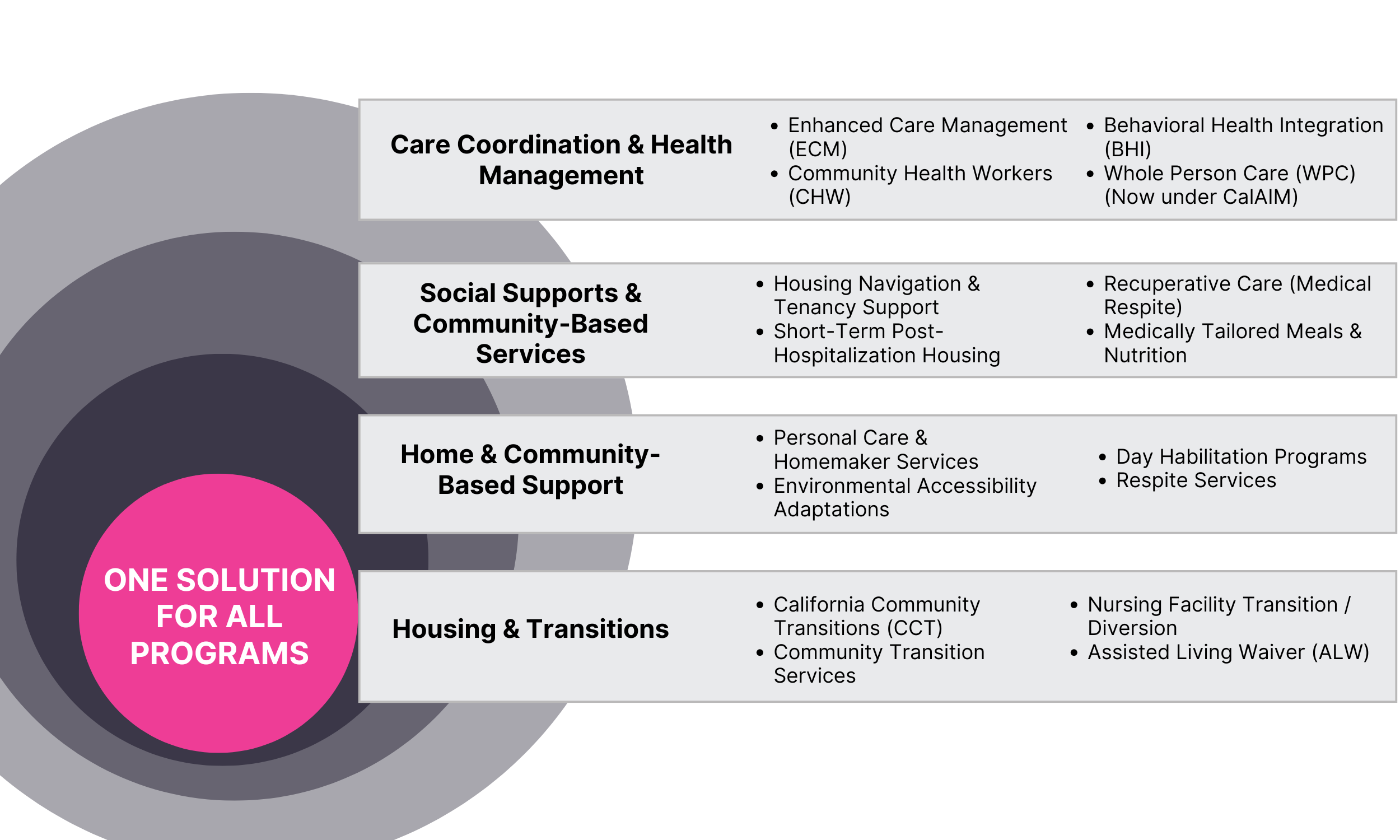
Challenges in Managing Multiple Programs: Many providers are responsible for delivering several CalAIM initiatives simultaneously, requiring braided funding strategies and seamless coordination【6】.
The Promise of CalAIM and Community Health Programs
Despite these challenges, CalAIM and community health programs have the potential to transform care delivery for vulnerable populations. These programs aim to:
Enhance Whole-Person Care: By addressing medical, behavioral, and social needs, providers can improve patient outcomes and reduce avoidable hospitalizations【8】
Expand Access to Non-Traditional Health Services: Programs like Community Supports (CS) offer housing navigation, food support, and in-home care to help stabilize high-risk individuals【9】
Support Value-Based Care & Financial Sustainability: Medi-Cal’s shift toward outcomes-based payments encourages data-driven decision-making to maximize reimbursements and efficiency【10】.
The various community programs, particularly those funded by Managed Care Plans (MCP), offer tremendous opportunities for CBOs to expand their services. Still, they also bring new complexities in claims processing, reporting, and compliance【12】.
How an Integrated Platform Transforms Community Health Programs
Aztute’s comprehensive, AI-driven community health platform is built to support organizations delivering ECM, CS, CHW, and other community-based programs. By integrating all services within a single ecosystem, providers can optimize efficiency, improve outcomes, and maximize financial sustainability【13】.
Seamless Enrollment & Integrated Referrals
Automates eligibility verification and member onboarding, reducing manual intake efforts.
Streamlines referrals between MCPs, CBOs, and BH providers for improved coordination of care.
Comprehensive Assessments & Whole-Person Care Planning
Conducts structured health and SDOH screenings to guide service allocation【14】.
Creates personalized, multi-provider care plans tailored to members' medical and social needs.
Optimized Service Delivery & Member Engagement
Tracks progress across programs, ensuring that interventions are timely and effective.
Provides telehealth, secure messaging, and mobile access for improved member engagement【15】.
Automated Compliance & Real-Time Reporting
Generates audit-ready documentation for DHCS, Medi-Cal, and MCPs, reducing administrative burden【16】.
Uses real-time dashboards to ensure compliance and optimize reporting workflows.
Billing & Reimbursement Optimization
Automates claims submission and reimbursement tracking, ensuring timely payments.
Supports funding braiding across Medi-Cal, grants, and other revenue streams to sustain programs【17】.
Interoperability & Data Sharing
Integrates with EHRs, HIEs, and MCP portals, enabling seamless data exchange.
Reduces duplication of effort, improving provider collaboration and efficiency【18】.
The Benefits of a Unified Platform for Community Health
✓ For Providers: One system to manage multiple programs, track compliance, and ensure financial sustainability.
✓ For MCPs & CBOs: Better coordination across organizations, real-time data exchange, and improved outcomes.
✓ For Members: Easier access to services, personalized care, and better health outcomes.
By implementing a fully integrated, technology-driven solution, organizations can streamline their operations, improve care coordination, and secure long-term sustainability in California’s evolving community health landscape. With automation, interoperability, and data-driven decision-making, providers can focus on what matters most—delivering high-quality care.
References
CalAIM Funding & Policy Changes: California Department of Health Care Services (DHCS) 2024 Budget Report
Proposed Federal Funding Cuts & Impact on Medi-Cal: California Budget & Policy Center, February 2025
Medi-Cal Budget Shortfall & Financial Risks: Politico, March 12, 2025
Administrative Burden in Community Health: California Health Care Foundation (CHCF) 2023 Report
Workforce Shortages & Increased Demand for Services: CalPERS, June 2024
Challenges in Managing Multiple Community Health Programs: Legislative Analyst’s Office (LAO) 2025 Report
Fragmented Data & Interoperability Barriers in Medi-Cal: Center for Health Care Strategies (CHCS) 2024
Impact of CalAIM on Whole-Person Care Outcomes: DHCS Evaluation Study 2024
Community Supports (CS) Expansion & Impact on Social Determinants of Health: California Health Care Foundation, 2024
Value-Based Payment (VBP) Model Implementation in Medi-Cal: DHCS Office of Health Care Affordability, 2024
Housing Support & Tenancy Services in Community Supports: National Low Income Housing Coalition, 2024
Community Health Workers (CHWs) & Their Role in Medi-Cal Programs: California CHW Workforce Report, 2024
Technology & Automation for Scaling Community Health Programs: Office of the National Coordinator for Health IT (ONC) 2024
Predictive Analytics & Risk Stratification in Member Health Management: Healthcare IT News, January 2025
Telehealth & Digital Tools for Medi-Cal Populations: California Telehealth Policy Coalition, 2024
Compliance Challenges in Medi-Cal Managed Care Programs: California Department of Managed Health Care, 2024
Financial Sustainability & Reimbursement Optimization in CalAIM: Medicaid Innovation Collaborative Case Study, 2024
Data Sharing & Interoperability Best Practices in Community Health Programs: California Health Information Exchange (Cal-HIE) 2024